Welcome back! As always, thanks so much for caring about me enough to tune in and read about the latest happenings. Today is the last day of my life without having gotten chemotherapy. So that feels weird. But it also somehow feels a lot like any other day. My sister being here this week has helped a lot with that. We’ve been staying busy working on the zen garden (I love it so much and she’s put SO much work into it), working on the workout garage space (also love it so much and again, she and my parents have put so much work into it), going for river and city park runs, enjoying funky little coffeeshops, catching up on class and work, going to doctor appointments, sharing fresh peaches from a farmstand, and spending too much time perusing plants at the nursery. Pretty much a perfect sisters’ week (well, minus the wine we would have at one point been sharing, but these days alcohol is certainly not the priority).
So I’m sure some people are wondering what the strange title of this blog entry means- it’s referring to the type of surgery I will likely opt for, which I’ll explain below. I had to steal it after my hilarious friend Ryan sent it to me after he learned of my intended surgical plan. I had my third of five meetings this morning with a breast surgeon, and I think I finally have some clarity about the route I’m going to take. The reason there are so many meetings is because with breast cancer, you essentially have a “deconstruction” surgery and, if you choose, a “reconstruction” surgery (and potentially a few in between for a variety of things). Because I am young and hopefully still have many years ahead, I will choose to have reconstruction done.
So, essentially you meet with a “deconstructing” surgeon, then usually meet with another for a second opinion, and same for the “reconstructing” surgeons (I’ll just type decon and recon from here on out because those words are far too long to continue typing over and over). So far I have met with a decon surgeon down at Anschutz who I really liked, but who will still be on maternity leave when I am likely to need surgery (late winter), so they’ll be referring me to another decon surgeon there to meet soon. I have a meeting with a recon surgeon down at Anschutz in late October, and I have met with both a decon and a recon surgeon here in Fort Collins at the Cancer Center. They essentially work in tandem, each specializing in different parts of the initial surgery, and then the recon surgeon comes back and does the later revision surgery alone. As I mentioned last week, it’s absolutely wild some of the things they can do and parts they can use for reconstruction. I’ve included a few photos here of cartoon depictions of the different areas they can get tissue, muscle, and fat from to relocate to the breast region to aid in volume and also in healing power.
In my case, since I am most likely opting for a double mastectomy for peace of mind that this doesn’t occur down the road in my right breast, and because I don’t plan to have biological children so I am not worried about breastfeeding, I have a few options that fall under the “immediate reconstruction” category:
- I could have both breasts removed with no autologous tissue put into either side (autologous tissue just means tissue, fat, or muscle from your own body), expanders put in for a few months, and then revision surgery to replace the expanders with implants 3-6 months after the initial surgery.
- I could have both breasts removed with autologous tissue put into just the left side (cancer side) from my latissimus dorsi muscle (aka the big side/back muscle used for things like tricep dips and pulling- known as the “lats”), and have the right side removed but instead of using the lat on that side, they use something called “ADM”, or acellular dermal matrix, as replacement for the breast tissue that’s been removed. Both sides would have an expander and later be replaced by implants (same time frame as above).
- I could have both breasts removed with autologus, latissimus dorsi muscle/tissue used on either side, expanders placed, and implants replacing the expanders at the same time frame as above.
- I could also go the route of using stomach fat or gluteal muscle/fat instead of my lat muscle, but the doctor said I’d have to eat a ton of pizzas before that would be possible and he didn’t recommend that during chemo treatment…plus I’m not really sure how I’d feel about taking muscle and fat off my bum to stuff it into my boobs (sorry for the visual, but hey, it’s weird and cool so I had to mention it).
- Side note: all of these would include removal of either just my “sentinel” lymph node or removal of multiple lymph nodes at the time of surgery. They do a biopsy of my node during surgery, and if it comes back positive for still having cancer in it, they’ll likely remove more- probably between 5 and 20- this is called an “axillary lymph node dissection”. If it’s negative for residual cancer, they then just remove the main affected lymph node (the sentinel) and do more radiation after the fact to try to reduce to potential for recurrence in any nodes.
There are a few advantages to the second option in italics- using my lat muscle/tissue on the left and the ADM on the right- the biggest one being related to radiation. Since I have to receive quite a bit of radiation to my left breast and axillary region for 6-7 weeks following the first surgery, and radiation really messes with skin and underlying tissue (think fibrosis, scarring, tightening, burns, etc.), the skin desperately needs good vasculature for blood flow and oxygen to the tissues to help it remain viable and heal. So, the lat muscle/tissue in that region really aids in healing and viability, and it lessens the chance of major damage to that area. Since my right breast won’t need radiation, it’s not necessary to do the lat muscle thing on that side. The ADM on that side will provide plenty of replacement for the breast tissue, and as long as my body allows it to heal as it should, I won’t need the enhanced support that the left side will need to aid in combating the forces of radiation.
As for the negatives, it obviously affects my lat muscle on the left side, and it’s a bigger surgery to recovery from, but he did say that many active, strong people who have this done go on to have minimal trouble with the affected side as long as they continue PT, working out, massage, acupuncture, etc. They do remove 1/2 to 2/3 of the muscle to move it around front, which again, is totally wacky, but he said people do really well. And it sounds like I’d have a really cool 23-cm scar just behind my current Western Hemlock tattoo along my left side, so he said I’d just have to get a second tree tattooed back there (which of course I will happily do, and my sister will get another matching tattoo, and we will finally convince Micah to get his matching sibs tree). So, I may never be great at tricep dips on the left side, and my upward dog may always be a bit crooked, but if it means better healing potential and reduced effects from radiation, I am down.

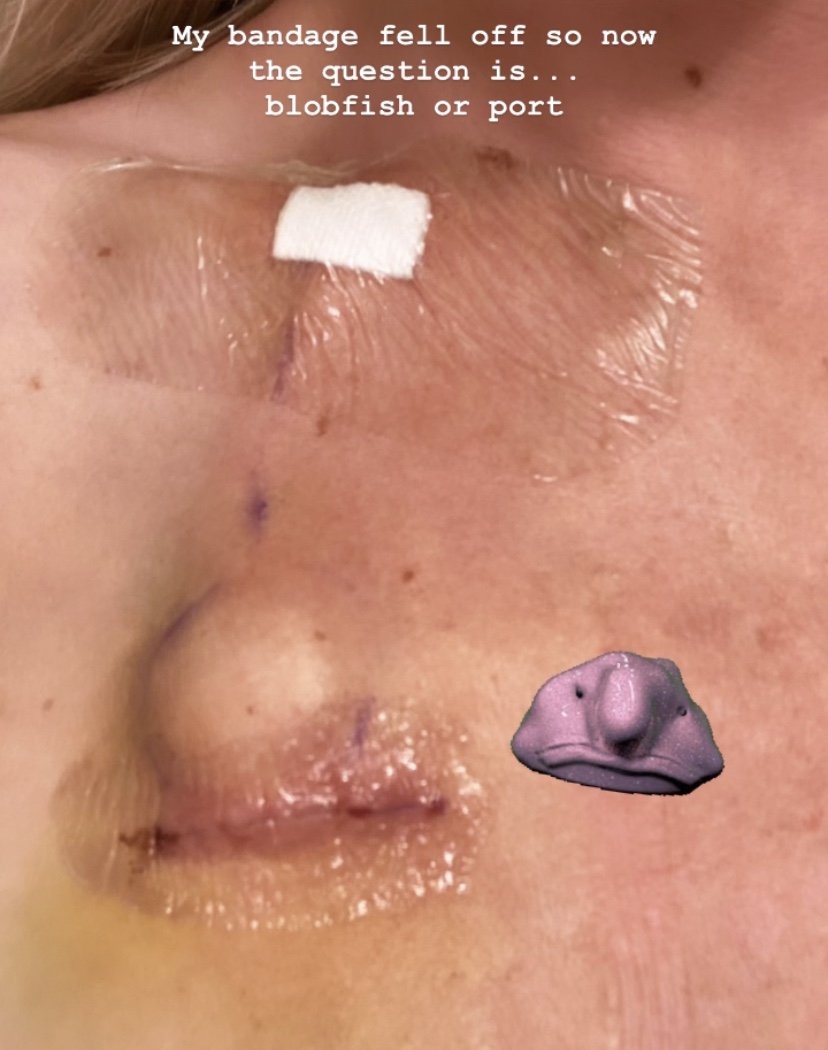
So, I’m probably going with the second option above. And in that case, I would have a literal side boob (for those of you who don’t get it, just know that my boob won’t actually be on my side).
One last thing to touch on is the different options for nipples- so many options for nipples! I couldn’t believe it. There’s nipple sparing, nipple-taking-away, nipple tattoos…so cool. A lot depends on whether the tumors are close enough to the nipple to determine whether it is “oncologically safe” to keep them and have them put on during reconstruction, or if there is a chance that there are cancer cells too close to the nipple that it’s safer to remove them completely and replace with nipple tattoos or not at all. I am still undecided on this part of it- I’ll likely just go with whatever the pathology report says when surgery time is closest. If it’s safe, maybe I’ll keep the pink ladies; if not, let’s toss them and I’ll get some sort of really cool half-sleeve-extending-across-the-chest tattoo (or maybe some amazing nipple tattoos).
Whew- so much info again. I hope this made some sort of sense. I think the biggest thing that’s been hard to stomach when meeting with these surgeons is that my reconstructive surgery (probably will take 3-4 different surgeries by the time it’s all said and done) will definitely extend into a year and a half or even longer from today. I likely will have to get the first big surgery in late winter- March or April 2022, then heal, then radiation for 2 months, then start my clinical year up again in the fall, get a few months of rotations and externships in, and then somehow figure out how to take time off to have reconstructive surgery done in the middle of 4th year (the “new” 4th year). So that’s going to be pretty rough, and I’ll still be on some level of chemo at that time (that’s a topic for another blog entry), and I’ll also be deciding whether or not to have a hysterectomy (uterus removed) during that timeframe as well. So, it’s a lot. But it’s also great to have options, and it’s wonderful to have so many people around me who know what I’ll be going through and who have been and I’m sure will continue to be understanding and patient as I navigate these decisions and what they mean for my future.
Ok, that’s all for now! Chemo starts tomorrow- my infusion appointment is bright and early and we will be there most of the day, so I’m sure I’ll have many more updates to come soon! Sending love and doggie kisses to all of you.